Bill Miller Arts
Bill Miller is an award-winning recording artist, performer, songwriter, speaker, painter, and world-class accomplished flute player. Over the past four years, Miller has produced three incredible albums, received a Grammy Award and led Wisconsin’s La Crosse Symphony Orchestra, a member of the League of American Orchestras.
Bill Miller has joined the NT Instruments team as one of the talented musicians that write content for the site, review several instruments and contribute overall to the growth of the site.
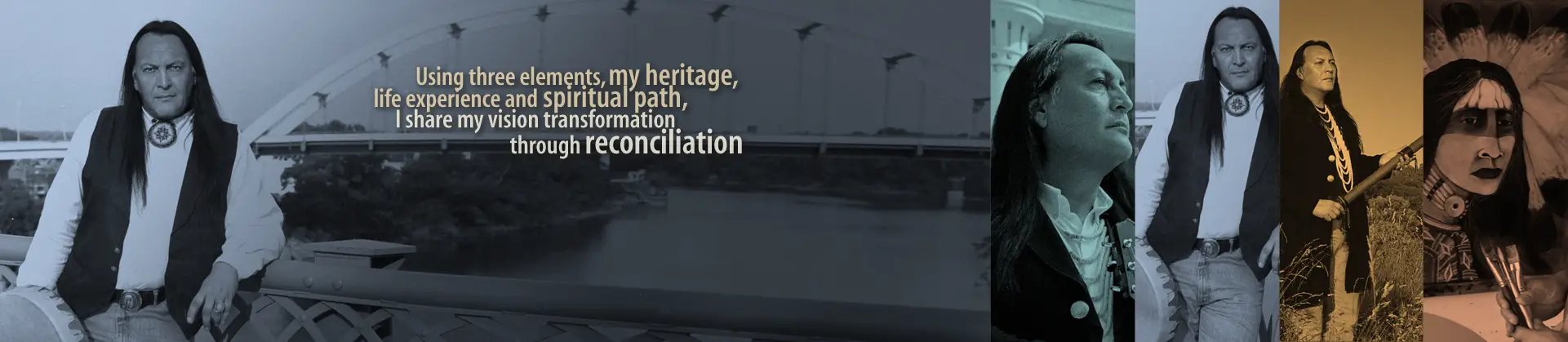
Whether painting a picture with his carefully chosen words or wielding a brush to place colors on canvas, Bill Birdsong Miller always creates from a vibrant emotional palette. Drawing from his own life experiences as well as centuries of tradition, Miller is an artist of considerable depth. A three-time Grammy winning singer/songwriter as well as an acclaimed speaker and gifted painter, Miller is the quintessential American artist. He has a restless creative spirit mingled with a well-grounded perspective and a heartfelt integrity that infuse his work with both substance and unique style. His artistry not only reflects his Native American heritage, but personifies the American experience.
Miller’s most recent work is Chronicles of Hope, a powerful collection of songs that simultaneously entertains and inspires. His musicianship, songwriting vision and vocal prowess coalesce brilliantly on this project. “I am a story teller,” Miller says. “I take notes on life, mostly my own, but others too. I observe situations. I listen in on people’s conversation. I interpret it in a musical way. I can’t help but do that.”
Miller’s list of accolades is lengthy and impressive. He has won six Native American Music Awards, including a 2007 Lifetime Achievement honor. He’s earned three Grammy Awards, among them his most recent in for “Spirit Wind North,” which was named Best Native American Album at the 2010 ceremony. He’s received international acclaim for “The Last Stand,” an original symphony he composed with Joshua Yudkin and Kristin Wilkinson. Some of the top names in the music community have sought out Miller as a collaborator, among them Michael Martin Murphey, Nanci Griffith and John Carter Cash, and he’s toured extensively, sharing the bill with a diverse slate of acts such as Tori Amos, Eddie Vedder and Arlo Guthrie. Well known for his beautiful performances on the flute, Miller was chosen to play flute on “Colors of the Wind” from Disney’s Pocahontas. As a painter, his work has been featured in the Smithsonian’s National Museum of the American Indian, the Trickster Gallery in Chicago, the Barbara Able Gallery in Santa Fe, and the American Indian Community House Gallery in New York.
More than the highlights on his professional resume, it’s his life experience that best defines Bill Birdsong Miller. A member of the Mohican tribe, he grew up in Wisconsin on the Stockbridge-Munsee Reservation in a home that combined the cultures of his Native American father with his mother’s German ancestry into a unique melting pot. “All I knew back then was the joy that music brought me. I think in those early days, there was a plan by God, my creator, that I would establish a relationship with music that was pure,” says Miller. “You’ve got to really recognize what something means to you before it becomes corporate, before it becomes taken for granted, when it truly is a joy and a gift.”
Growing up in a turbulent home with an alcoholic father, music was a means of emotional escape for Miller. “My father really wasn’t there for me. He was struggling with his alcoholism,” Miller says. “With an alcoholic father, the way I could escape was by putting myself in my music and my art. It helped me through everything. Music was pure joy, yet I didn’t think of being a musician. What I wanted to be was a visual artist. I drew and painted at a young age, and I won a scholarship out of high school into art school. I was really going to be a painter or an art teacher.”
Though he couldn’t see it at the time, Miller’s difficult childhood was shaping his future and the impact he would eventually have on others. Refusing to let his past be an anchor that drug him down, Miller learned to move from victim to victory and has encouraged others to do the same. “Now if I were to look back, there’s a master plan of how I was being set up to be a reconciler and it’s taken me this long to accept that responsibility. It’s a big responsibility because I’ve still got traces of my dad in me,” he says quietly. “I had a lot of anger issues. You can’t go through a life like that as a child on a reservation with a violent alcoholic father and not have anger issues. It all affected me and today it comes down to recognizing who I am, what I am, what I stand for and what I’m about. It’s like a compass. My compass points true north and true north is reconciliation. True north is about sacred ground. True north is knowing what things mean to me and really not going away from that.”
After high school, Miller began attending the prestigious Layton School of Art and Design in Milwaukee and began performing locally while he was also painting and pursuing his degree. He met pop star turned country performer Michael Martin Murphey following a concert and Murphey was so impressed, he called his agent the next day and booked Miller as his opening act. The two artists forged a friendship that remains strong to this day.
Miller became one of the principal performers at West Fest, a series of festivals Murphey created to celebrate the culture and heritage of the West. It was Murphey and Miller’s friends in the Nitty Gritty Dirt Band that encouraged him to move to Nashville where he and his wife, Renee, have made their home for more than 20 years, raising their three biological children and adopting another son and a wheelchair-bound daughter with spina bifida.
Miller has become one of the Nashville community’s most respected talents, working with Vince Gill, John Carter Cash and other Music City luminaries. He has recorded nearly 20 albums—both as an independent artist and for Warner, Integrity, Vanguard and other labels. Much of his time has always been spent on the road. “I’ve been on the road for so long and you’d think it would get ugly now or old, but I’m actually more invigorated by the road and the journeys and the stories,” he says. “I’m more excited than I was before because I really believe now that I have a purpose, not to say that I didn’t know that I had a purpose, but back then I was pursuing a record deal, and even getting it, I was in pursuit of other things. Now I’m in pursuit of excellence. I’m in pursuit of reconciliation. I’m in pursuit of music that supports that and I’m having the joy of my life with my family.”
Not bound to one creative medium, Miller continues to paint as well as make music. “Those two worlds work well together and it’s a great way for me to express myself,” he says. “I don’t see it as any less a gift than music. I used to put all my efforts into music, but now I do put a lot of time into my art. I like to create images that speak, same as my music. I want people to walk away and remember that image. That’s not easy to do. I did my cover for this last album that won a Grammy ‘Spirit Wind North.’ That’s my painting. I just love to paint and I want to spend more time doing it.”
As if Miller’s schedule wasn’t already full enough, he’s also a highly sought after public speaker. “It’s another platform for me because I’m not afraid to talk to anybody or in front of anybody. I speak on reconciliation and how reconciliation makes a difference in your world,” says Miller, who has been asked to address executives at AIG, MTV, FDIC and the Environmental Protection Agency.
He’s also looking for additional opportunities to expose “The Last Stand,” which commemorates the Battle of Little Big Horn of the Great Sioux War of 1876-77. The symphony, which took Miller and friends four years to write, has been performed in Israel by the Kibbutz Orchestra. Miller accompanied playing the Native American flute and guitar. “It was unbelievable,” he says. “ I was so looking forward to it and it was more than I ever dreamed of. The people there accepted it with tears and open arms and ovations. They were very blown away by it. They related to it. I think it was the perfect place to do it.’
He’s also looking forward to hitting the road again to share new music from Chronicles of Hope. “This is the most unique record I’ve made in the years because it was delving into life and death issues. I didn’t plan it to be that way, but the songs became prophetic,” he confesses. “I went through a lot of life lessons.”
Chronicles of Hope is Miller’s most personal, most transparent work to date. “This was the most freeing record because it was like a journal to me. On ‘The Last Breath’ it talks about how you could be seeing this or breathing it for the last time. I was writing about myself as well as the world’s issues, asking ‘What does this land mean to me? What does my marriage and faith mean to me?’”
Taking his own personal observations and experiences and creating art that is universal in its ability to strike people in the heart—that has long been Bill Miller’s gift. Whether the medium is painting, music or the spoken word, Miller is a communicator. It’s his heritage and his future, intimately intertwined, and rarely has someone used that gift more passionately or effectively than this Native son.
Contents
Awards
Three–time Grammy award-winning songwriter and musician: Best Native American Music Album, “Spirit Wind North” –2010, “Cedar Dream Songs” –2004, “Sacred Ground–A Tribute to Mother Earth”–2005. Winner of seven Native American Music awards: Lifetime Achievement –2007, Song of The Year, and Single of the Year -2006, Best Male Artist, Songwriter of the Year, Folk Artist of the Year, Single of the Year, and Song of The Year for “Ghost Dance” –1999.
TV Appearances
NBC–Today Show with Katie Couric, CNN-Showbiz Today, PBS–Austin City Limits,PBS–Special “Songs of the Spirit”, RFD–TV, PBS-Special “For The Generations”
Syndicated Radio Performances and Interviews
NPR–Washington, D.C., WSM Radio, XM Radio, Woodsongs Radio Hour, Mountain Stage Radio.
Art Showcases
“The Trail of the Painted Ponies–“Ghost Horse,” Santa Fe New Mexico Gallery showings include: Fort Hayes Shot Tower Gallery–Columbus, Barbara Able Gallery–Santa Fe, Trickster Gallery–Chicago, American Indian Community House Gallery–NYC, Koshare Indian Museum, La Junta, CO
Speaking Engagement Highlights
The Smithsonian Institution’s National Museum of the American Indian–NYC, AIG Corporation, MTV Networks–NYC, Environmental Protection Agency–Washington D.C., FDIC Headquarters–Washington D.C., Universities and colleges nationwide, Community and recovery centers nationwide
- Viola vs Violin – 5 Key Differences Between The Two Instruments - March 20, 2024
- 15 of the Most Famous Violinists of All Time (18th Century to Present) - March 20, 2024
- Full School Band Instruments List (Elementary / Middle / High) - March 18, 2024
